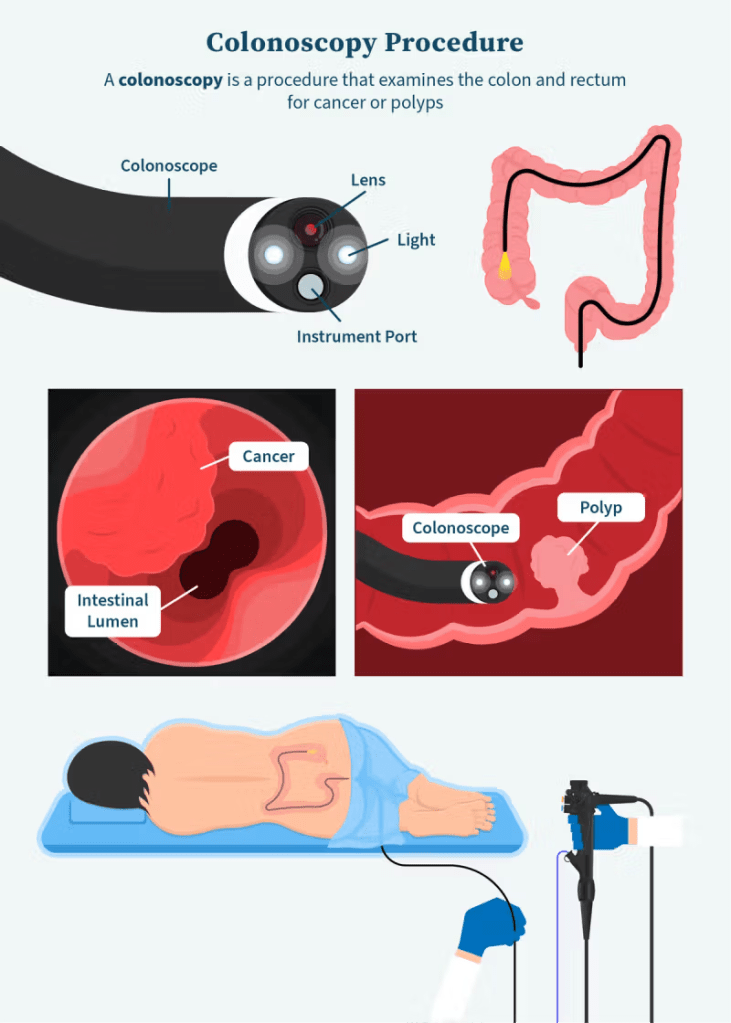
Colonoscopy or coloscopy is a medical procedure involving the endoscopic examination of the large bowel and the distal portion of the small bowel. This examination is performed using either a CCD camera or a fiber optic camera, which is mounted on a flexible tube and passed through the anus
The last time I had one of these was in 2008. I was in hospital in Cork with what I thought was a kidney stone but following a CT Scan my consultant referred me to a Gastroenterologist (GI) within the hospital. This specialist had only been appointed to the hospital so he was travelling back and forth to the UK. Basically he advised the ward doctor to commence a 72 hour infusion of a strong antibiotic. I was not permitted to eat or drink throughout these 72 hours.
I was in the surgical ward with 3 other patients in the room, when the doctor decided to visit me. His first words were “You’ll be on a stoma (colostomy bag) for the rest of your life”. My answer was “No I won’t” This conversation had started badly… he responded with “There are no options here. I need to operate and remove a substantial amount of your colon” seriously how to piss someone off within seconds.. “You haven’t even examined me yet so, no you will not be going near me in surgery”… Our voices were raised but before he could respond a lady that was visiting another patient spoke up “ That is a disgraceful way to speak to a patient !” he turned and looked at her and asked “Are you a patient here? And she answered “No I am visiting my husband, but I have only recently retired after 30 years in nursing” he looked her straight in the face and told her to GET OUT pointing at the door. Anita was outside in the ward speaking to the Ward matron. They heard every word and Anita suggested to the Matron to intervene as she could hear that my temper was about to go. The Matron entered the room and asked the consultant to come out to discuss this in private with her. Anita entered the room and asked me to relax. To be honest I was definitely seeing RED and ready to batter this ignorant git. But I did simmer down, the Matron returned and asked if I was okay and I said yes but told her not to let that doctor back near me. I lifted my mobile and called a consultant I had met in Dublin to make an appointment to see him. I informed the Matron that I was meeting a specialist later that week in Dublin and I needed a copy of the CT Scan to take with me, she went out and called my urologist that had admitted me. I was handed the phone by the Matron.
Basically the Consultant Urologist was not happy, he told me that I was too ill to travel to Dublin and needed treatment as soon as possible, I explained that I did not want the surgeon anywhere near me and basically requested to be discharged under advice immediately. So I handed the phone back to the Matron who eventually removed the IV line and called radiology to get a copy of the CT Scan.
And with that I left the hospital and travelled to Dublin that afternoon to meet with the consultant the next day. Talk about a completely different attitude, this man was a complete gentleman, he did a physical examination and then read the Radiologist report. He booked me in for the following day for a colonoscopy with the option to be lightly sedated or fully sedated. I decided on fully sedated. He then took the CT Scan DVD and said he was sending it to his team to examine it. I left the hospital and headed to my Mums house (She lived in Dublin). Bright and early the next morning I was back at the hospital and admitted to a day ward. The Consultant met me and advised that under full sedation I would need to be in hospital all day as against light sedation where I would be discharged an hour later. I still opted for full sedation.
I was linked up to an IV and prepped for surgery. I had an agreement with the consultant that he could not operate on me and this was clearly noted on the consent form. I was taken to the surgical unit and sedated. I’m not sure how long after that I was awoken by the consultant “Everything is fine”
Everything is fine! Now I was confused. How could the consultant in Cork diagnose acute diverticulitis with an urgency for surgery. This consultant said it was mild not acute diverticulitis and no intervention was necessary. He had done a number of biopsies which would take about a week for the results to be ready but discharged me saying that I needed to have a scope every 5 years.
My Dad had passed away in 1994 due to Colon cancer and I needed to keep an eye on my own colon as it is classed as hereditary, but only at about 10%, The consultant also mentioned that they had examined the DVD of the CT Scan and could not find any issues.
That was 2008 “Doctors differ” I have not had another scope since. My oncologist felt that they would see any issues in the scans over the course of my cancer treatment. Up to 2024 all CT Scans showed a low level of diverticulitis. But in Feb 2024 prior to my official 5 year all clear the Oncologist had ordered a high definition CT Scan, I had left the hospital and was close to home some 120klm from the hospital and my mobile went it was my oncologist. He asked where I was and I told him, he told me to return to the hospital as soon as possible as it appeared that my colon was close to rupturing and required urgent medical intervention. He said he was referring me to the consultant I had met in 2008 and I instantly said no. I got home and explained the situation to Anita and that I had an appointment the following week with the Oncologist anyway and could discuss it further with him.
February 2024, I met my oncologist for my 6 month review and my 5 year remission update. And yes I was all clear but he did explain the risk of acute diverticulitis with a warning that if the colon ruptured then it would be life threatening. We were in the process of buying a house some 250klms away so he added a recommendation on his report to my new GP about organising a colonoscopy. He also placed me on an antibiotic to settle the current inflammation.
Almost 16 years since I had the meeting with the specialist and no serious issues, no bag and happy that I didn’t let him near me. But by September 2024 I felt it was now necessary to get the long overdue colonoscopy and met my GP to have them organise it. The diverticulitis attacks were becoming more regular and took longer to clear.
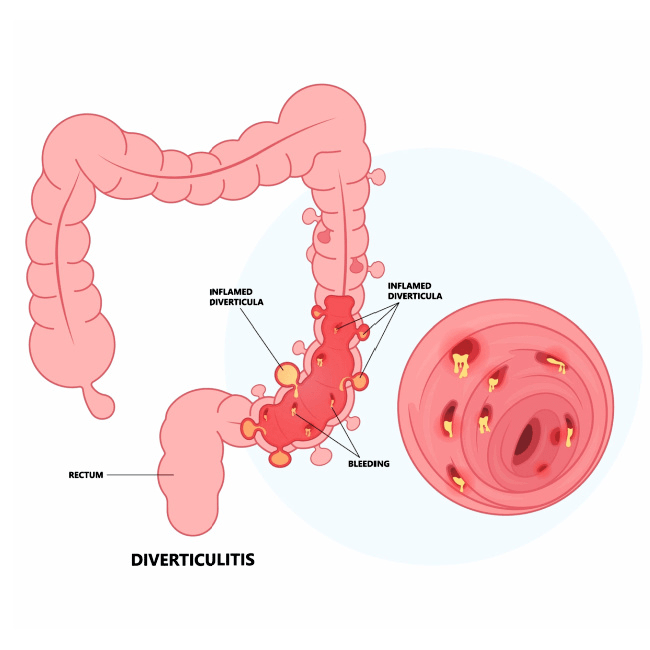
Diverticulitis – Diverticulosis occurs when small defects in the muscle of the wall of the large intestine or colon allow small pockets or pouches (diverticula) to form. Diverticulitis is infection or inflammation of these abnormal pouches. Together, these conditions are called diverticular disease.
The GP sent a referral letter to the nearest hospital with a red tag (this is a priority note of referral and only a letter to A&E would be higher) I had opted for the referral to be red tagged as the closest A&E was about 45 minutes away and I wanted time to stabilise myself for the procedure.
Blood test markers associated with my continued remission from lymphoma we’re being thrown off by the recurring Diverticulitis, one of the main tests ESR (erythrocyte sedimentation rate ) and white blood cell count were very high but my oncologist considered this to be my immune system fighting Diverticulitis.
Two weeks ago I got the procedure date as 19th of November and received the prep prescription the next day in the post. The prep is basically a laxative to clear out the colon so the scope can access the entire length of the colon.
14th of November- 5 days to go and I went to the pharmacy to get the necessary prescription. Only to be charged €24 for it, I’m a medical card holder, this basically covers my GP cost and monthly prescriptions. I’ve had this card since 2014 and it was an absolute battle to get. In Ireland we have public healthcare that covers a lot but we also have private health insurance which I have had since leaving college, it’s not cheap but it gives you access to private hospitals. All the chemotherapy was done inside a private hospital but the Stem Cell Transplant was in a public hospital (cost covered by the state). Between the public cover and private cover is a grey area, NTAP scans, MRIs and consultant fees are not covered unless you’re admitted overnight these scans and meetings really add up, hence the estimated personal cost of €25,000 over the past 10 years. I was lucky enough to get a personal loan in 2016 and only finished paying it off a few months ago. It is challenging to paying for your life. But if I didn’t have private healthcare I’m not sure if I’d be alive today.
I got a call from the hospital in the afternoon, initially I thought it was just to confirm everything but it was actually them cancelling. The doctor in charge of my procedure also works for another hospital and she had to cancel the clinic due to over booking in her other practice. The earliest next appointment would be late January 2025. I asked if there was another GI that they could refer me to but I got a “no sorry” and advised to call my GP to have them refer me to a different hospital. The call ended and I contacted my GP, the colonoscopy was arranged through the National health service HSE so I requested the GP to arrange it privately in the hope I would get this done soon. I’m still waiting for the GP to get back to me. I am in the middle of another diverticulitis attack so I hope to have an answer soon.
We are in a government election year and expect a lot of local politicians to knock on our door, I’m looking forward to confronting them with their manifesto for healthcare in Ireland.
I am still classed as Stage 4 Multiple Lymphoma, my families medical history includes Colon Cancer, both my Oncologist and my GP have red tagged a colonoscopy as urgent.
This can be a life threatening situation especially if the damaged area of the colon ruptures as the crap (literally) leaking into my body could most likely cause Sepsis .
If you go into any clinic or hospital in Ireland there are warning signs on their boards about the risk of Sepsis and the need for urgent medical treatment
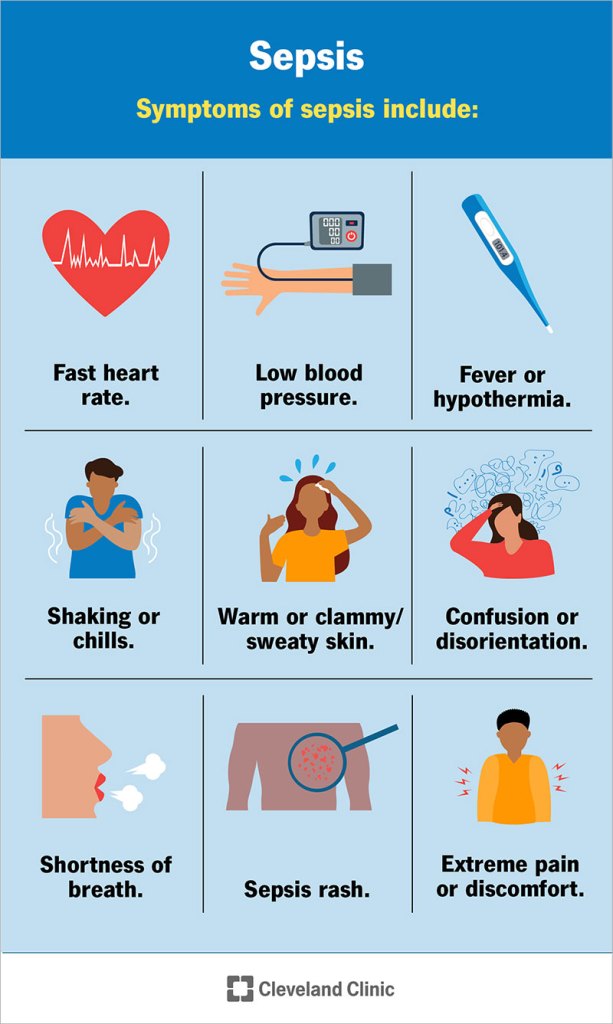
Sepsis is a serious condition that happens when the body’s immune system has an extreme response to an infection. The body’s reaction causes damage to its own tissues and organs.
Sepsis can affect anyone, but people who are older, very young, pregnant or have other health problems are at higher risk.
Common signs of sepsis include fever, fast heart rate, rapid breathing, confusion and body pain. It can lead to septic shock, multiple organ failure and death.
Sepsis is usually caused by bacterial infections but may be the result of other infections such as viruses, parasites or fungi.
Update 16/11/2024
I now have a private appointment in Bons Secours Galway for the 27th of November ….
And a new date set for 27th under private medical insurance my national health insurance would have meant waiting till January. The prep for the procedure started on the 24th with two tablets to help empty the colon. This part of the update I am writing is on the 25th of November, a day I seriously dislike, my Dad passed away 30 years ago today. He had been diagnosed with right side Colon cancer in August 1994 the tumour has been missed on scans and was only discovered during exploratory surgery. His body rejected the chemotherapy – it is amazing the amount of progress that medical science has made over the last 30 years. The medical approach has also changed thankfully and it is better focused on dealing with a cancer diagnoses to the victim and their families. Back in August 1994 the surgeon that operated on my Dad phoned my Mum at home and told her over the phone that he had 3 to 6 months to live – I lived in Cork some 160 miles away, that call was at 10pm I arrived in Dublin 3 hours later to get to my Mum, we had not expected cancer so the shock to my Mum was unreal. We met the consultant the next day and I nearly went through him but he found my approach completely unacceptable, how times have changed. All I got as a response your father has 3 to 6 months left to live and the former is properly closer and by the way it is hereditary with males. I suppose at the time the research values were not perfected like today, the reality is that the chance of hereditary is at 10% with a 5% risk of inherited gene changes (mutations). But it also shows the poor judgment by a professor – why not tell a son that what he will see happen to his father would most likely happen to him. My Dad had just retired that year at 65. It was a year where I had made two new friends through work. At the time I was a Logistics consultant working with Memorex Telex where I had the absolute pleasure of meeting Rachael, who is still a friend to this day. And a man from a transport company that went on to be a business partner from the following year but that friendship ended suddenly when I relapsed in 2017. In my father’s case they never confirmed where the cancer originated but had concluded that his liver and colon were most likely.
Like my sister I still struggle with the memories of those 3 months, sitting watching our dad slowly fade away.
So in the build up to this scan I am nervous because of a seed that was planted in my brain 30 years ago by a doctor. I have been through 2 terminally classed battles against Cancer in 10 years and I really don’t want to commence a war against cancer again.
26th November 2024
The day before the colonoscopy, I commenced reducing food intake two days ago and today I have to take the flush out medication. The first of two at midday and the mixture had a taste of Mango off it. You have to drink 500 ltrs of this over an hour and yes it does work. Within minutes I was visiting the toilet. 2 hours late the second mix is consumed but this one has a different taste and much more sever. Over the next couple of hours I must have lost about 5kgs in weight. All I had to eat all day was clear soup. I felt that I had successfully cleared out my colon.
27th November 2024 Colonoscopy Day
Anita travelled with me as I would not be permitted to leave the hospital alone nor could I drive for 24 hours following the procedure. Weather was very poor, with a heavy fog and -5 temperatures’ so I drove down to the hospital roughly an hours drive. We got there a few minutes late but the staff fully understood the road difficulties. Anita dropped me off and took the car so she could go shopping locally and I entered the admissions. I was told that I would be next to undergo the procedure and was taken to the day ward. The consultant came out to chat to me about the procedure and I requested only partial sedation. I explained that I wanted to see the area damaged in the colon and if there were any other issues.
I would say that I was only in the unit an hour before they moved me into the procedures room.
It’s a strange feeling to be able to see the inside of your body on a screen a few feet away. The doctor explained that he needed to remove a few polyps
Colon polyps indicate a protrusion of the mucosa which may have a cancerous or a non-cancerous character. Age has a vast influence on the onset and development of polyps. Below 30 years of age polyps occur only rarely, but with increasing age the risk of disease rises as well as the number and the size of polyps. The larger the number and the size, the higher the risk of developing a polyp into a malignant tumor. It is therefore very important to prevent and monitor polyps and their timely removal. Colon polyps are tricky due to their asymptomatic growth.
This was not unusual and they were mostly small. These polyps were to be send like a biopsy to confirm wether or not there were cancer cells present.
But as the specialist entered the Sigmold Colon an area that was declared as close to rupture in Feb It appeared clear and only mild divititculious. Again it appeared that the radiologist had over reacted following my CT Scan in Feb.
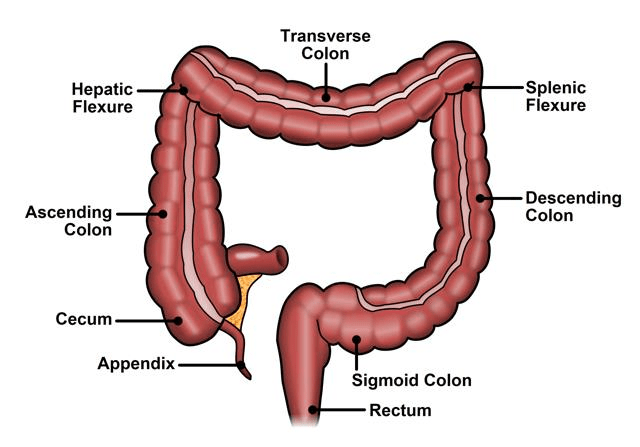
And I am sure the doctor noticed the sigh of relief from me, Yes it looked a little raw but nothing close to seriously damaged. He did remove a polyp in this area that was large and I watched intensely as he looped a wire around the base of the polyp and basically snipped it, he them retrieved the polyp which will be sent for analyzes (that can take a few weeks). He then proceeded further up the colon and into the Ascending Colon. The right side colon called the Ascending Colon is where my dad’s tumour was and to see this as clear was very relaxing for me.
After the procedure was completed I was moved to the recovery area. The staff in this ward are very easy going but very professional. I was made a cup and toast. I really needed the tea as I was fasting from midnight. About 20 minutes after the tea I was asked to call the person that was collecting me. I had to sign the discharge paperwork which included a 24 hour no drive instruction. Before leaving the hospital the consultant came over to me, he remarked that the procedure went well and that the colon “clearout” was good, he advised that I had mild Diverticulitis that could become painful but could be managed with prescription medication and diet and no further medical intervention was necessary . He removed 6 polyps all would be sent to be analyzed and the results would be back in a week or two. He handed me a number of copies of the report for my GP and my oncologist. Prior to the procedure they did do a blood sugar test (this was due to my history with diabetes) the reading was a little higher than expected at 8.5, I now need to start home testing again to insure that this is not a flare up. I will have another colonoscopy in 12 months and then every 5 years pending the results of the biopsies.
And with that we headed home. As per the doctors instructions I spent the rest of the day in bed and decided to take it easy for the next 24 hours. The relief of knowing that my colon was not going to rupture and that the colon appeared clear is great. Just another test to add to the multitude over the past 10 years.
Dear Ian, thank you for writing this blog.
Isn’t it amazing how listening to our own, deepest instinct and body are life saving ?
LikeLike